By Niklas Moeller
In order to comply with the speech privacy requirements established by the Health Insurance Portability and Accountability Act (HIPAA) in 2000, hospitals are increasingly installing sound masking to address scores related to the quietness of patients’ rooms at night.
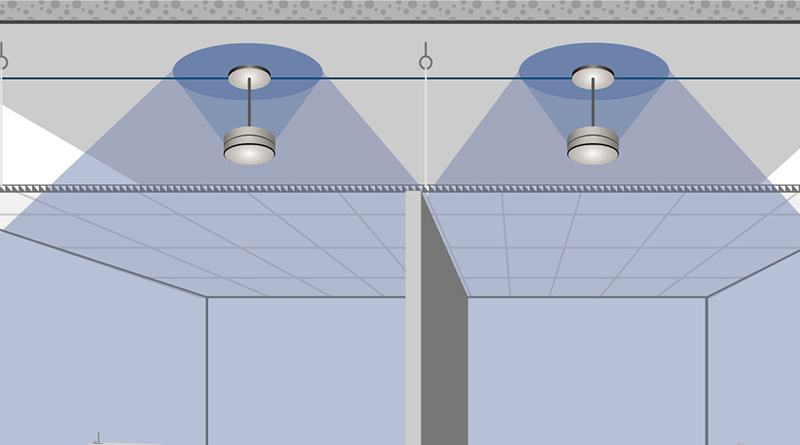
This technology uses loudspeakers to distribute an engineered sound throughout the facility. While adding sound might appear to contradict the goal of controlling acoustics, the new ambient level covers up noises that are lower in volume while reducing the disruptive impact of those that are higher by minimizing the degree of change occupants experience. Similarly, conversations are entirely masked or their intelligibility is reduced. Therefore, occupants perceive treated spaces as quieter.
Unlike ‘white noise’ or ‘pink noise’— terms often, but incorrectly, used in this context — sound masking follows a non-linear spectrum or ‘curve’ specifically designed to balance acoustic control and occupant comfort. A successful implementation achieves both goals, in equal measure. However, no sound masking system can accomplish these objectives out of the box.
The sound produced by sound masking changes as it interacts with various elements across the facility’s interior, such as the layout and furnishings. In order to ensure the system provides the intended effects and that they are enjoyed equally by all occupants, an acoustician or trained technician must tune the sound so that it meets the specified curve across the entire treated area. To do so, they measure the sound at ear height, examine the results, and adjust the system’s volume and frequency settings accordingly. They repeat these steps as often as needed at each tuning location until the measured output meets the target curve.

Photo Credit: K.R. Moeller Associates Ltd.
Ideally, the target curve should be provided by an acoustician or a third-party such as the National Research Council (NRC), rather than by the system’s manufacturer or vendor. As perfection is impossible to achieve across the entire treated space, the specification should also include a ‘tolerance’ indicating by how much the sound is allowed to deviate from that curve. However, because variations in the masking sound can significantly impact speech privacy, noise control and occupant comfort, this value should be kept to a minimum.
In order to achieve such consistency in the highly fragmented environment of a hospital, the sound masking system should be designed to offer small control zones with fine volume (i.e., 0.5 dB steps) and frequency control (i.e., third-octave) within each one. Each closed room should be an independent zone, while open plans should be covered by control zones no larger than three loudspeakers each, allowing the acoustician or technician to make precise, local adjustments across the entire space.
In order for future changes to be made without re-opening the ceiling — which can spread microbiological contaminants, as well as dust, fibers and odors into the occupied space below — the system should provide control over all settings from a central location. Ideally, patients should also be given control over the masking volume within their own room, using a keypad, rotary knob or app. An administrator ought to be able to establish upper and lower limits for these controls.
Niklas Moeller is vice president at K.R. Moeller Associates Ltd.